Complex tasks. Simple execution.

Administration Portal
Wellvation collaboratively designs ManageWell’s Administration Portal to simplify the complexities that come with delivering personalized wellness programming.


Workflow and analytics are intelligently automated to:
- Match programming to each employee’s confidence and risks.
- Know what works and where to improve.
- Continually updated to stay innovative and relevant.
Admin Resources
Simplify administration while personalizing experiences
Complex tasks made simple.

Segment participant groups
Segment participant groups
From couch potatoes to triathletes, meet participants wherever they are and help them get to the next level using Mayo Clinic resources.

Communicate with participants
Communicate with participants
Never lose a participant due to irrelevant, generic communications again.

Leverage insurance claims data
Leverage insurance claims data
Define and automate eligibility file uploads and transfers, edit records, and manage day-to-day tasks.

Manage any incentive strategy
Manage any incentive strategy
Match any and every combination of incentives to your organization and participants’ goals.

Optimize programming with AI
Optimize programming with AI
Artificial intelligence technology continuously adapts to increase personalization, automate execution, and accelerate impacts.

Real-time, on-demand reporting
Real-time, on-demand reporting
Visualize program impacts, opportunities, and value propositions for your organization’s participants.

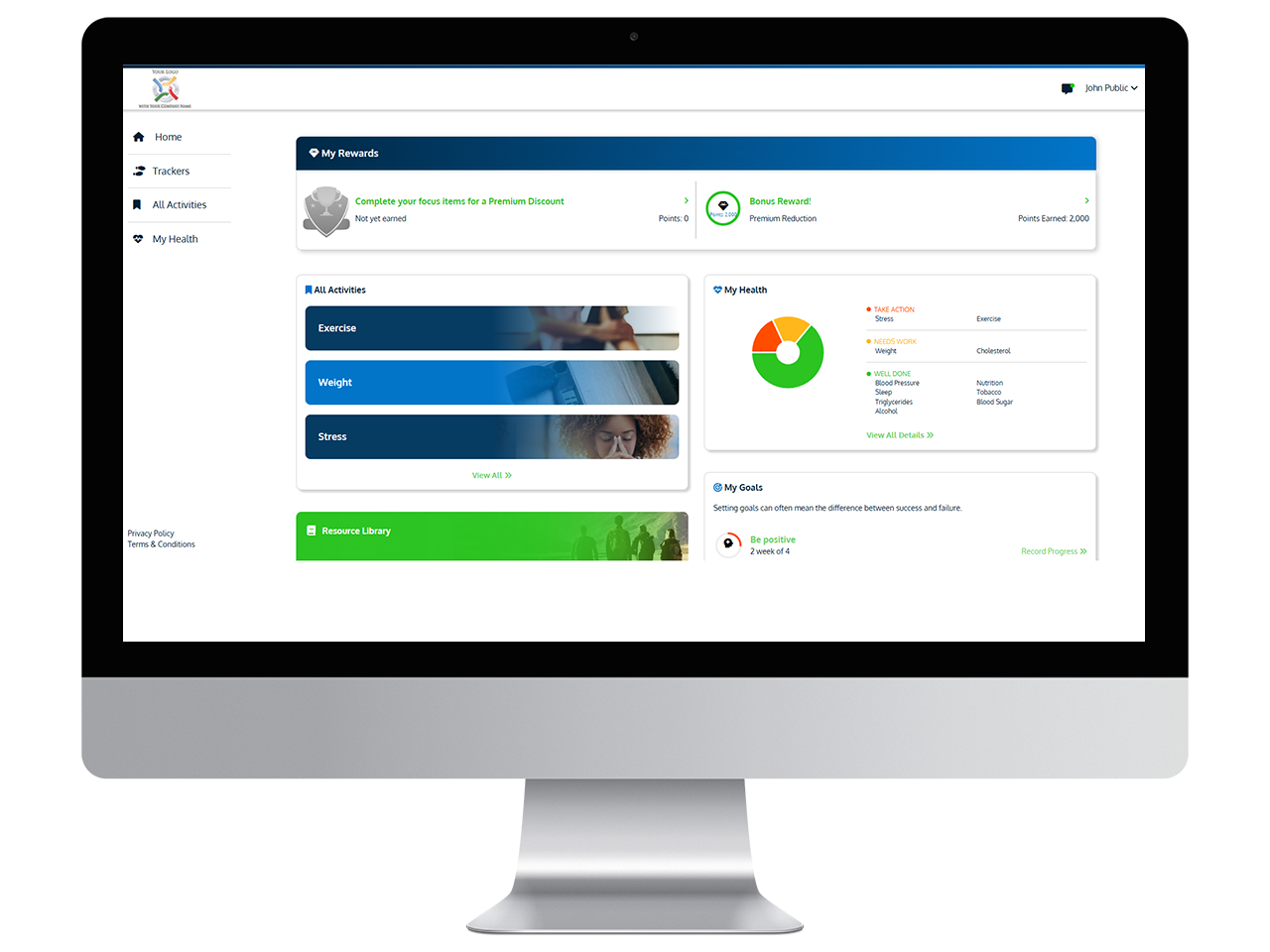
Having the right goals is important, but those goals aren’t going to do you any good without a plan in place to achieve them.
Wellvation meets the needs of consumers by providing them with trusted health information by Mayo Clinic and engagement with wellness tools and resources, utilizing a systematic approach that leads to sustainable improvements in their health.
Personalization is extremely important because everyone has different goals and challenges. What works for one person may not work for another. Personalizing your plan so that it’s truly yours makes it much more likely that you’ll be successful.